COBRA & California Cal-Cobra
Federal & Cal COBRA
Federal COBRA and California Cal-COBRA basically provide that if you are no longer covered “qualifying event” under your Employer’s group health plan, you can keep the group coverage regardless of your health and with no pre-existing condition clause for 18 (Federal) or 36 months (California) at 2 to 10% more premium than your employer was being billed from the Insurance Company.
Qualifying event examples:
-
losing your job, regardless of if you were laid off, fired or passed away.
-
your child lost his student status, gets married, no longer a dependent or reached age 26
-
Divorce or a spiteful spouse who took you or children off the policy… even though CA Divorce Law Financial Automatic Restraining Orders FL 110 prohibits financial changes. 26 CFR 54.4980B-4 Qualifying Events *
Since everything now is Guaranteed Issue with No Pre-X under Health Care Reform, consider going on an Individual Plan (Get Quotes). Even if it’s NOT Open Enrollment, there is Special Enrollment, as you have just lost coverage MEC Minimum Essential Coverage. Under Special Enrollment, your coverage is the first of the month after you apply, rather than the crazy 15th and miss a month deadline. Emails dated 1.21.2015 2:07 PM
If you have problems obtaining your COBRA, or CAL COBRA coverage, we can lead you in the right direction. There is no such place as Cal COBRA. It’s a law that guarantees you can keep your employer’s group plan when you terminate employment. It’s basically though something that you arrange directly through your Former Employer’s HR Department or Insurance Company. (SB 719, California Continuation Benefits Replacement Act §10128.50 et seq. , §1366.2, AB 1401 )
We suggest that you get Quotes and see if you can get a better alternative than COBRA. Not all members of the family have to take COBRA for one member to get coverage. With your own Individual coverage you have the option of taking a higher deductible, HSA Health Savings Account get quotes on dental, life or vision to save $$$.
#Options for getting coverage when you lose your job?
- Cal Cobra & Cobra
- Don’t worry about getting notified… You will and you will have time to make a decision!
- Private Coverage – Direct or Covered CA with Subsidies – NO Medical Questions – No Pre X
- Medi – Cal Medi Cal does monthly qualification too!
Learn More – Links & References
- FAQ’s on right to keep Employer Plan
- VIDEO Losing Job-Based Coverage
- Continuity of Care same doctor even if no longer in network
- Department of Managed Health Care on COBRA & Cal COBRA
- Check out your Evidence of Coverage – Actual Policy for rules & procedures
-
Department of Managed Health Care on COBRA & Cal COBRA
-
Disability Benefits 101 FAQ’s Cal COBRA
-
Pit Falls of Cal COBRA – DI 101
-
DOL (Dept. of Labor) More Info – Job Loss
- Our webpage on Continuity of Care
- Legal Match.com enter your problem, issue or summary of case and interested attorney’s will contact you.
- Our webpage on Registered Domestic Partners – Spousal Health Coverage?
-
F. Medicare And Other Health Insurance Coverage Hi Cap CA Health Care Advocates
FAQ’s
Mandatory #Notification of COBRA & Cal Cobra Rights
When there occurs a “qualifying event” that entitles persons covered by an employer group health plan to elect continuation coverage, such as the employee’s termination of employment or death, the divorce of the employee and his or her spouse, or a dependent child’s ceasing to qualify for dependent coverage under the plan, a notice of the right to elect continuation coverage generally must be sent to each person (termed in the COBRA law a “qualified beneficiary”) who has that right.
If the “qualifying event” is the employee’s termination, reduction of hours or death, the employer has 30 days after the event (or, if later, 30 days after the date coverage is lost) to notify the plan administrator, which in turn must give the notice of COBRA rights within 14 days to persons entitled to elect coverage. (If the employer and the plan administrator are the same, it has the full 44 days to give the notice.)
How soon the notice is provided affects how long eligible persons have to elect continuation coverage because they must be given at least 60 days from the date of the notice. Wilcox & Savage Esq. * Reporting & Disclosure Guide (DOL) California Cobra Program [10128.50 – 10128.59]
Get more detail in the Employees Guide to COBRA page 5
excerpt from the Blue Cross Employer Administrative Manual page 36:
You [Mr. Employer] are required by law to allow eligible employees to remain on the plan until their employment is terminated. The termination will be effective the first of the month following the last day of employment.
When can COBRA rates to go up?
The applicable premium must be fixed for a 12-month “determination period.” ERISA § 604 (3); Treas. Reg. § 54.4980B-8, Q/A-2(a) §1164 (3). Therefore, a mid-period increase in insurance rates will not permit a mid-period increase in the COBRA premium charged to QBs. Heart of Matters.com benefitslink.com/
The law limits the conditions when the applicable premium may be increased during a determination period.
A determination period is any 12-month period selected by the plan that is applied consistently from year to year. During a determination period, a plan can increase the premium only in the following three cases:
- (1) The plan has previously charged less than the maximum amount permitted and the increased amount required to be paid does not exceed the maximum amount permitted; or
- (2) The increase occurs during a disability extension and the increased amount required to be paid does not exceed the maximum amount permitted; or
- (3) A qualified beneficiary changes the coverage being received. Because the law is clear in its guidance for premium increases, it is advisable to consult your benefits professional or legal counsel when passing on rate increases to COBRA participants for reasons not stated above. (cobrapoint.com)
When your COBRA rates change, you can get a special enrollment into an individual plan.
You can get coverage within 60 days of losing COBRA without having to wait for open enrollment special-enrollment-triggering-events/
Lapse? Re-Instatement? Grace Period? COBRA
There is a minimum 30-day grace period for each successive payment due date. Payment is considered made on the date it is postmarked (if it is mailed), not the date of the check or the date the payment is physically received by the Plan. (cms.gov Page 15 Section V # 4, dol.gov, vantaggiohr.com Treasury Regulation §54.4980b-8 Question # 5)
Under the new regulations, qualified beneficiaries must receive what is called an “Early Termination Notice” if they lose coverage due to failure to make payment by the due date or within the grace period. (dol.gov/)
Gross Misconduct?
Gross Misconduct Might prevent you from getting COBRA. It’s not defined in the code, thus
Courts that have faced the gross misconduct case generally refer to the two questions below when deciding if the conduct is truly gross misconduct.
- Was the conduct intentional, willful, deliberate or reckless, and was that conduct performed with a conscious or reckless disregard of the consequences of one’s acts for the very purpose of causing harm or with knowledge that harm would result in the employer’s best interest?
- Did the conduct have a connection or series of connections or physical presence linking the gross misconduct or performance directly to the employer, a co-worker or a current or former client or customer? East Coast Risk Management * HR Service Inc *
Steve's VIDEO introduction to Cal COBRA
- Instant Health Quotes & Enroll
- 15 Reasons to appoint us as your broker - No extra charge
- VIDEO - Moving from Employer Plan to Individual Plan
- Department of Labor VIDEO on COBRA and various other rights
Employee’s guide to #COBRA –
Department of Labor
- EmployER's Guide to COBRA
- DOL on Health & Retirement benefits after job loss
- DOL on COBRA
- Legislation to make COBRA credible coverage
- FAQ CA Department of Insurance
- CA Department of Managed Health Care FAQ's
*********
Art Gallagher Employers Guide to COBRA
- Our Webpage on COBRA & Cal COBRA
- Get Individual Guaranteed Issue ACA/Obamacare Quotes -
- Subsidies if you make less than 600% of Federal Poverty Level!
- No Pre X Clause!
- No wait for Open Enrollment as you get Special Enrollment when you lose COBRA or your Employer Group Plan!
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services

Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
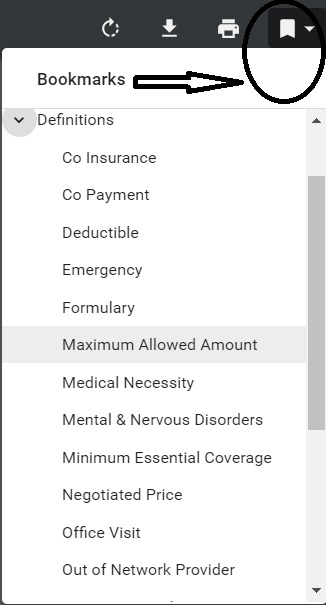
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.
VIDEO Steve Explains how to read EOC
FAQ’s
- COBRA doesn’t count as Active Employer Coverage to give you a special enrollment period to Medicare A & B.
- I’m getting benefits as a part time employee, rather than full time and pay a higher contribution rate. I haven’t met the 90 day probation period to get full benefits. waiting-period Do I qualify for COBRA?
- We need to see a copy of your ID Card and your Evidence of Coverage to provide an authoritative answer, rather than a SWAG one.
- We are concerned that you might not have a GROUP plan but possibly a individual temporary plan that might not qualify as a group plan. See pages 2, 4 & 5 in Employee’s Guide to Benefits under COBRA.
- A qualified beneficiary is an individual who was covered by a group health plan on the day before a qualifying event occurred that caused him or her to lose coverage.
- Under COBRA, a group health plan is any arrangement that an employer establishes or maintains to provide employees or their families with medical care, whether it is provided through insurance, by a health maintenance organization, out of the employer’s assets on a pay-as-you-go basis, or otherwise. “Medical care” typically covered by a group health plan for this purpose includes:
- • Inpatient and outpatient hospital care;
- • Physician care;
- • Surgery and other major medical benefits;
- • Prescription drugs;
- • Dental and vision care.
- See page 5 of Employers Guide to COBRA for more details on notices, including letting you know when you first get covered under the Employer Plan that COBRA rights are included when you lose coverage.
- 2 Penalties are on these other websites SHRM.com * Bizfluent.com * Queens Employment Attorney.com
Out of State? #Self Insurance?
If you worked for an Employer who was headquartered Out of State, they do not have to offer you the additional 18 months of Cal Cobra coverage after COBRA or even the original 36 months, of Cal COBRA, if they are a small employer. CA Law Definition Employer * (§10128.53) and not subject to Federal COBRA. That’s a mouthful isn’t it. Please double check it, before relying on it.
The CA Insurance Code shall not apply to a policy… that covers hospital, medical, or surgical expenses and that is
-
issued outside of California
-
to an employer whose principal place of business
-
U.S. Supreme Court has held that, absent unusual circumstances, a corporation’s principal place of business is its nerve center, i.e., the place where its officers direct, control, and coordinate the corporation’s activities Cornell Law * Nixon Peabody and
-
-
majority of employees are located outside of California. (§10112.5(b) *
It’s possible that your Employer might be in CA, but is owned by a larger company, headquartered out of CA and thus they may not have to offer Cal COBRA.
Since everything now is Guaranteed Issue with No Pre-X under Health Care Reform, consider going on an Individual Plan,
Even if it’s NOT Open Enrollment, there is Special Enrollment. Under Special Enrollment, your coverage is the first of the month after you apply, rather than the crazy 15th and miss a month deadline. Emails dated 1.21.2015 2:07 PM
The 36 months of Cal COBRA coverage does not apply to self insured health care plans that are covered by the Employee Retirement Income Security Act (ERISA).disability benefits 101.org Metropolitan Life Insurance Company v. Massachusetts, 471 U.S. 724 (1985), the U.S. Supreme Court ruled that state laws governing self-insured benefit plans are subject to ERISA preemption. Foley & Lardner Attorney Analysis
http://www.cvtrust.org/ is one of the state’s largest self-funded PPO public schools’ trust Since they are self funded the trust comes under the “self-funded or insured” exemption in the webpage above.
What happens if my EmployER sells the business?
Does the NEW owner have to cover my COBRA?
Simply put, the answer is YES, even if it’s just a sale of assets. See details and examples in the Code of Federal Regulations § 54.4980B-9
See our webpages on:
Term Life Quote #naaipquote
- Set up Schedule a phone, skype or face to face consultation
- Tools - Calculator to help you figure out how much you should get
Life Insurance Buyers Guide
How much life insurance you really need?

Please complete & return
- Short ONE page form - CPS
and we'll search and consult for you.
FAQ’s
- Question My Employer contributions for my Health Care Plan ended when I turned 65. Under a special enrollment period, we applied for coverage under my husbands government retirement plan. My original plan covered me, my husband and my disabled dependent daughter age 28. My spouses group insurance is denying my request to enroll my daughter – citing that she needed to be continuously enrolled (with them) beginning at the age of 26. This appears to be a discrimination under HIPPA or ERISA. I am wondering if I should proceed to a fair hearing.
. - Answer We deal with this issue of changing insurance companies here If you have additional questions, please ask there.
. - Question I was employed by a 200 person company for 4 years and had Anthem Prudent PPO group insurance. I went on to Cobra after leaving the job, and paid the full premiums. Six months later, the company went to a self-insured plan still offering Anthem Prudent PPO.
- 1) Is there any grandfather clause or law that would allow me to get Ca lCobra since I was already on Cobra before the change to self insured was made?
- 2) Can they simply refuse to offer Cal Cobra even though I was told in email it would be offered to me because I was already on Cobra before the change?
.
- Answer I’m not aware of any grandfathering provision that would make an Employer Offer Cal COBRA if the employer goes out of business, moves to a self insured plan or simply stops offering Medical Insurance. There has to be an Insurance Plan for the COBRA to “come from.”
- Under Health Care Reform, you can get an Individual Policy regardless of your health status – pre-existing conditions, at the same rates as everyone else. You may even qualify for subsidies. Get a FREE quote here.
- If you still insist you want Cal COBRA, try following the links above, but I doubt it. nahu.org NABIP/looking-for-an-agent Outside of California
#Service In Network Area
- Once you move out of the service area, the geographical area where you can get Covered Services from an In-Network Provider, CA Law Website * double check your evidence of coverage for exact rules in Plain English, you wouldn’t be able to continue COBRA or Cal COBRA dmhc.ca.gov *
- When Cal-COBRA Continuation Ends.
- The date the Insured moves out of the plan’s service area or commits fraud or deception in the use of services. eoc.hospital.plus.
****************- (k) “Service area” means a geographical area designated by the plan within which a plan shall provide health care services. leginfo.legislature.ca.gov
**** - A geographic area where a health insurance plan accepts members if it limits membership based on where people live.
For plans that limit which doctors and hospitals you may use, it’s also generally the area where you can get routine (non-emergency) services. The plan may end your coverage if you move out of the plan’s service area. .healthcare.gov/
*********** - A coverage area (also called service area) is a specific region where a health insurer’s members can get covered care under their plan. The insurance company contracts with doctors, medical groups, pharmacies, and hospitals in this area to guarantee in-network rates for its members. For EPO or HMO plans, you have to live within a coverage area in order to sign up for an insurance policy. hioscar.com/service-area
********* - Service Area: The geographic area served by an insurer or healthcare provider. glossary
- (k) “Service area” means a geographical area designated by the plan within which a plan shall provide health care services. leginfo.legislature.ca.gov
- In-Network Provider Definition
- A Provider that has a contract, either directly or indirectly, with us, or another organization, to give Covered Services to Members through negotiated payment arrangements under this Plan.
- FAQ’s
HISTORICAL
H.R.1319 – American #Rescue Plan Act of 2021
FREE COBRA for Six Months!
Subtitle F–Preserving Health Benefits for Workers
Under section 9501, qualifying COBRA enrollees would be required to pay 15 percent
Note – all the interpretations say nothing
of the total COBRA and Cal COBRA premium from the first of the month following the date of enactment through September 30, 2021. The federal government would provide a subsidy on behalf of the individual for the remainder.
People would be eligible for premiums to be paid on their behalf [So, as I understand it, the employer pays the premium and gets a credit on their payroll taxes] if they are enrolled in, or are eligible to enroll in, COBRA or Cal COBRA coverage because of an involuntary termination or reduction of hours at the time of enactment. Section 9501 would permit eligible people who did not previously elect COBRA coverage and eligible people who discontinued COBRA coverage prior to enact CBO *
SEC. 9501. PRESERVING HEALTH BENEFITS FOR WORKERS.
(A) Reduction of premiums payable.–In the case of any premium for a period of coverage during the period beginning on the first day of the first month beginning after the date of the enactment of this Act, [April 1st 2021] and ending on September 30, 2021, for COBRA continuation coverage with respect to any assistance eligible individual described in paragraph (3), such individual shall be treated for purposes of any COBRA continuation provision as having paid in full the amount of such premium.
(B) Plan enrollment option.–
(i) In general.–Solely for purposes of this subsection, the COBRA continuation provisions shall be applied such that any assistance eligible individual who is enrolled in a group health plan offered by a plan sponsor may, not later than 90 days after the date of notice of the
plan enrollment option described in this subparagraph, elect to enroll in coverage under a plan offered by such plan sponsor that is different than coverage under the plan in which such individual was enrolled at the time, in the case of any assistance eligible individual described in paragraph (3), the qualifying event specified in section 603(2) of the Employee Retirement Income Security Act of 1974, section 4980B(f)(3)(B) of the Internal Revenue Code of 1986, or section 2203(2) of the Public Health Service Act, except for the voluntary termination
***See our Q & A on definition of voluntary termination
of such individual’s employment by such individual, occurred, and such coverage shall be treated as COBRA continuation
coverage for purposes of the applicable COBRA continuation coverage provision.
(3) Assistance eligible individual.–For purposes of this section, the term “assistance eligible individual” means, with respect to a period of coverage during the period beginning on the first day of the first month beginning after the date of the enactment of this Act, and ending on September 30, 2021, any individual that is a qualified beneficiary who–
(A) is eligible for COBRA continuation coverage by reason of a qualifying event specified in section 603(2) of the Employee Retirement Income Security Act of 1974, section 4980B(f)(3)(B) of the Internal Revenue Code of 1986, or section 2203(2) of the Public Health Service Act, except for the voluntary termination of such individual’s employment by such individual; and
(A) In general.–The Secretary of Labor, in consultation with the Secretary of the Treasury and the Secretary of Health and Human Services, shall provide outreach consisting of public education and enrollment assistance relating to premium assistance provided under this subsection. Such outreach shall target employers, group health plan administrators, public assistance programs, States, insurers, and other entities as determined appropriate by such Secretaries. Such outreach shall include an initial focus on those individuals electing
continuation coverage who are referred to in paragraph (5)(C). Information on such premium assistance, including enrollment,
shall also be made available on websites of the Departments of Labor, Treasury, and Health and Human Services.
(B) Enrollment under medicare.–The Secretary of Health and Human Services shall provide outreach consisting of public education. Such outreach shall target individuals who lose health insurance coverage. Such outreach shall include information regarding enrollment for Medicare benefits for purposes of preventing mistaken delays of such enrollment by such individuals, including lifetime penalties for failure of timely enrollment.
(9) Definitions.–For purposes of this section:
(B) Cobra continuation coverage.–The term “COBRA continuation coverage” #means continuation coverage provided pursuant to part 6 of subtitle B of title I of the Employee Retirement Income Security Act of 1974 (other than under section 609), title XXII of the Public Health Service Act, or section 4980B of the Internal Revenue Code of 1986 (other than subsection (f)(1) of such section insofar as it relates to pediatric vaccines), or under a State program that provides comparable continuation coverage. Such term does not include coverage under a health flexible spending arrangement under a cafeteria plan within the meaning of section 125 of the Internal Revenue Code of 1986.
“SEC. 6432. CONTINUATION COVERAGE #PREMIUM ASSISTANCE.
“(a) In General.–The person to whom premiums are payable for continuation coverage under section 9501(a)(1) of the American Rescue
Plan Act of 2021 shall be allowed as a credit against the tax imposed by section 3111(b), [Employment Taxes] or so much of the taxes imposed under section 3221(a) as are attributable to the rate in effect under section 3111(b), for each calendar quarter an amount equal to the premiums not paid by assistance eligible individuals for such coverage by reason of such section 9501(a)(1) with respect to such calendar quarter.
“(3) in the case of any group health plan not described in paragraph (1) or (2), the insurer providing the coverage under the group health plan. Congress.Gov *
Resources & Links
- FAQ’s from Blue Cross
- Summary from CBO Cost Estimate
- LA Times Summary
- LA Times – Free COBRA
- Word & Brown Summary
- Blue Shield Summary
- Covered CA Seminar 4.20.2021
- Cal Choice – Introduction
- FAQ’s
- DOL.Gov on COBRA Subsidy
- Sharp Health Plan FAQ
3rd Party Administrators & Reference Services
BROKER ONLY
Brother - Sister - Sibling Side Pages Subpages
View our website with your Desktop or Tablet for the most information


I am an employee who took an early retirement (age 57) from a company that I worked for in MA, and I signed up for COBRA upon my separation.
I moved to CA a month later.
Will I be eligible for CAL-COBRA at the end of 18 months of Federal COBRA?
The company I worked for also has a presence in CA (I was transferred from CA to MA 4 years ago), and my COBRA health plan is available in CA.
Please see the law above about the requirements for when California has jurisdiction to make a plan offer Cal COBRA.
Do you still think your MA Employer is subject to the Cal COBRA requirements?
Rather than trying to interpret complex law, how about sending us your EOC Evidence of Coverage.
How about a brand new, guaranteed issue individual plan – get a quote.
Transfer FED COBRA to CAL COBRA
my Federal cobra insurance at Kaiser expire 11/30/21, and I would like to apply CAL cobra Kaiser.
Please let me know who or whom can help me.
thank you
How about getting an ACA/ObamaCare/ARPA quote here with possible subsidies?
Contact your former employer’s HR Department
Kaiser Tool to help you determine what works best for you.
If it’s a Kaiser Individual Plan, check our webpage on that.
I have a company that is sitused in CA with a CA based dental plan. An ex-employee that lives in MN continues the dental benefit through COBRA Continuation.
Is the ex-employee able to continue the dental benefit through CalCOBRA after the 18 months is over?
10128.53.
(a) Every disability insurer, that provides coverage under a group benefit plan to an employer, including those policies and contracts that provide vision-only and dental-only benefits, as defined in Section 10128.51, shall offer continuation coverage, pursuant to this section, to a qualified beneficiary under the contract upon a qualifying event without evidence of insurability.
Steve,
Your professional advice and suggestion are really appreciated.
Thanks!
can you give me a simple explanation as to why I’m being told by my former employers HR department that once we started Cobra, we’re locked into until January?
They weren’t able to tell me anything that sounded sensible, and yet they seemed very sure of themselves.
I’m not a mind reader, so I really can’t tell you why someone said something… I could try to make an educated guess.
The real issue is not what they said, but if you are still within 60 days of losing employer coverage, can you get a special enrollment for losing coverage into ACA/Obamacare, right?
Here’s Blue Shield’s rule in simple English. You have 60 days from when you lost employer coverge to get an ACA/Obama Plan. Get quotes here. If you want a complex answer you can find the actual codes here and follow the relevant links. Is there anywhere that it says you lose the 60 day right, if you pick the “wrong” plan?
Guessing why your prior employers HR department said you have to wait till January?
They don’t want to be bothered setting up COBRA if you’re going to cancel it right away. You should have done the shopping around first.
It’s a lot more work for us too! Plus, under ACA/Obama we practically have to pay the insurance companies to get them to take your policy. If you weren’t a prior preferred client, we’d tell you just to stay with COBRA as we’ve spent too much time to make a piddly commission. How many other professionals in this business can make an analysis and explanation like this?
You have 60 days to enroll in COBRA
You now have coverage and generally you can’t cancel and change till Open Enrollment. See the code on our webpage for special enrollment loss of coverage
Loss of coverage can’t be your voluntary cancellation. So, your HR dept figures you have coverage and you can’t cancel. We say, your special enrollment is 60 days and the loss is due to job ending. Put that on your application. If you put that you cancelled COBRA, the HR department is correct.
Probably 95% of the people that call and want to cancel are beyond 60 days.
When is your employer’s Open Enrollment? Is it also January?
Is there confusing with the Employer’s Cafeteria plan rules? You’re no longer an employee, right?
Did they read the law 3 times and then when they think they understood it, read it again?
Even if by chance the HR department is correct, what do you have to lose completing an application? Just click add to cart when you get the quotes.
Does the ACA/Obama application ask if you had COBRA?
What was the question you asked them?
Did you ask, if I want to change when can I do it?
or did you ask if I have a 60 right to special enrollment after losing employer coverage?